Spiking sugars. Falling sugars. Long-term complications. Diabetes can get between you and a fulfilling sex life. Our experts dish on the benefits and common issues of sex (and how to solve them), the conversations to have with care providers, and thought about Diabetic Living
1 – Communicate openly about what you’re feeling. Take your attention off the glucose levels for a while; you might consider wearing CGM. It helps with spontaneity.
2 – “Apply a sense of humour,” is Roszler’s suggestion. “It helps you both laugh off the challenging moments.”
Long-term, years of glucose swings along with risk factors such as excess weight, cigarette smoking, and uncontrolled blood pressure and lipids can take their toll, including on sex organs.
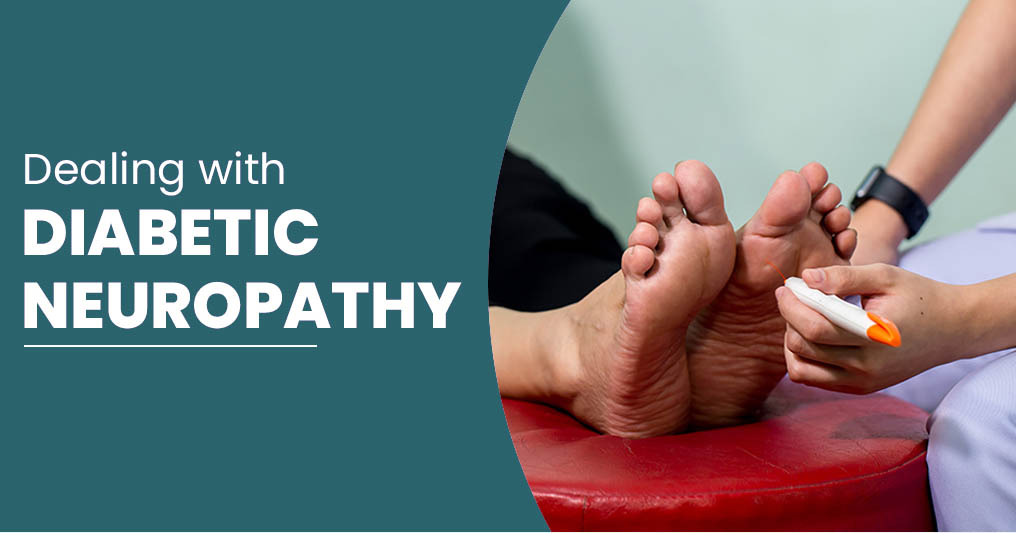
Circulatory and nervous systems play lead roles here. A form of diabetic nerve disease called autonomic neuropathy damages nerves that manage automatic functions, from controlling blood pressure to digesting food and, yes, the behaviour of your sex organs. Then there’s blood flow. If it’s hampered, you might not receive enough blood below the belt to get aroused.
3 – Glucose control and healthy lifestyle choices can greatly reduce these issues. Good sex offers a bevy of benefits, from the physical to emotional, so it’s worth the effort, says Dr. Rupin Shah. “Sex is a key ingredient for a happy life that allows us a deeply meaningful level of trust and belonging.”
BEYOND THE BOUDOIR
These are the most common issues, tests and treatments for sexual issues in PWD.
WOMEN Potential problems:
Female sexual dysfunction includes loss of sexual interest or desire, difficulties with arousal, lack of lubrication, painful intercourse, and inability to reach orgasm. Diabetes, nerve and circulation problems, ageing, menopause, frequent yeast infections and depression all increase the likelihood of dysfunction.
Checks and tests:
Candidly share with your provider gynaecological and sexual history (past and current partners) and diabetes control. Mention all meds. And be honest about alcohol, drugs and tobacco use. Though it can be tough, be straightforward and open. Your provider will do a pelvic exam to check for physical changes.
Today’s treatments:
“Providers typically start with the least expensive and easiest strategies with a proven track record,” Roszler says. These include moderate weight loss
(if needed), physical activity, healthy eating, minimal alcohol use, stress reduction and better glucose control.
Create an open line of communication with your partner. Your doctor may recommend a mental health provider or sex therapist to help, as well as vaginal lubricants to aid dryness or pain.
If these don’t help, you may explore other options: localised vaginal estrogen in a ring, cream or tablet, or other hormone treatments.
MEN Potential problems:
The major male sexual problem is erectile dysfunction (ED): the inability to achieve and maintain an erection. At least half of men who have lived with diabetes for 10 years or more experience ED.
This may start before other complications, or it may be the initial symptom of diabetes.
“A related problem is andropause, the age-dependent decrease of the male hormone testosterone, which experts increasingly associate with loss of erectile function,” says Shah.
Low T, as it’s called, is also referred to as ‘male menopause’.
Checks and tests:
To diagnose ED, your provider will go through similar personal, sexual and medical histories as for women. Be straightforward and open. Next up, they may suggest blood work to measure
testosterone, thyroid and other hormones, as well as other tests.
Today’s treatments:
Start with the same lifestyle habits and actions for diabetes control that are recommended for women. Your health care provider may also try medication to help improve blood flow in the penis to achieve better erections.
Common TGA-approved meds are Viagra (sildenafil), Levitra (vardenafil), Stendra (avanafil) and Cialis (tadalafil). But men with significant heart disease and circulatory issues get a red flag. “Significant can be defined as enough to trigger a heart attack or stroke,” says Krongrad.
Sex isn’t typically a cause of heart attack or stroke, but ED can signal heart or circulatory problems, so tell your doctor.
Other treatments for ED include penile injection therapy, surgical implant of a penile prosthesis, or a vacuum device. Include your partner in the talks and come to a decision together.
Hormones and blood sugar:
Just as diabetes affects sex, a woman’s periods may affect her management.
“Hormone changes can affect glucose control,” says Aimee Gallagher, scientific program manager for the Society for Women’s Health Research.
Note glucose level changes over each cycle. Perimenopause and menopause can also create new glucose patterns – for example, an early sign of menopause for women on insulin is low blood sugar caused by dropping progesterone levels.
“Stay active, practise good sleep habits, and check glucose often to make sure that menopause symptoms are not high or low glucose,” Gallagher says. “They can mimic each other.