Some pregnancies will be classified as high risk, that is why it is so important to visit your doctor when you decide you want to have a baby or realise you might be pregnant.
And once you have been told it is high risk, as a mother you want to know if things will be okay, and what to do to minimise the risk.
If you have a high-risk pregnancy you are at increased risk of health problems before, during and after delivery.
Read More: How to choose the best pregnancy test
It is therefore important that you are registered with your doctor for antenatal care services, including classes.
Your provider will advice you to start taking a daily prenatal vitamin with folic acid and ensure you reach a healthy weight before you become pregnant.
If you have a medical condition, your treatment might be adjusted in preparation for pregnancy. Your health-care provider might also discuss your risk of having a baby with a genetic condition.
Go to your regular antenatal visits to have your health and your baby’s health monitored.
You might be referred to a specialist in cases where problems are detected early enough. This is most important, especially for people who have had previous pregnancy complications, including miscarriages.
Avoid risky substances. If you smoke, quit. Alcohol and illegal drugs are off-limits, too. Talk to your health-care provider about any medications or supplements you’re taking.
Read : 7 Benefits Of Eating Fish During Pregnancy
Causes of a high-risk pregnancy
A high-risk pregnancy may be due to illnesses or medical conditions that you had before you were pregnant, or medication that you have been taking all along.
It may happen however that you develop certain conditions during the pregnancy that will cause the pregnancy to be classified as high risk.
The following factors will cause a pregnancy to be high risk whether there is an illness or not:
Lifestyle choices. Smoking, drinking alcohol and using illegal drugs.
Advanced maternal age. Pregnancy risks are higher for mothers older than age 35.
High blood pressure, obesity, diabetes, epilepsy, thyroid disease, heart or blood disorders, poorly controlled asthma, and infections can increase risks.
Multiple pregnancy. Pregnancy risks are higher for women carrying more than one foetus.
Pregnancy complications. Examples include a placenta not in the right position in the uterus, a baby not growing as they should, and rhesus (Rh) sensitisation – a potentially serious condition that can occur when your blood group is Rh negative and your baby’s Rh positive.
Previous pregnancy complications. A history of pregnancy-related hypertension disorders, such as preeclampsia, increases risks.
If you gave birth prematurely in your last pregnancy, or you’ve had multiple premature births, you’re at increased risk of an early delivery in your next pregnancy.
Talk to your healthcare provider about your complete obstetric history.
Symptoms of high-risk
Vaginal bleeding or watery vaginal discharge; Severe headaches;
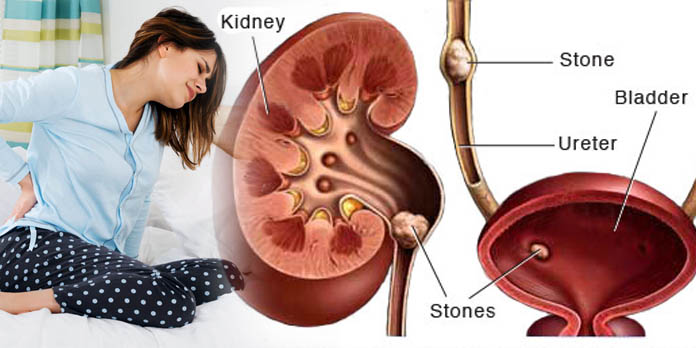
Pain or cramping in the lower abdomen; Decreased foetal activity; Pain or burning with urination;
Changes in vision, including blurred vision;
Sudden or severe swelling in the face, hands or fingers; Fever or chills; Vomiting or persistent nausea; Dizziness; and Thoughts of harming yourself or your baby.
Tests to use
The most important first is history-taking and physical examination.
Your doctor or nurse will go through your past pregnancies, your general health and lifestyle.
Then do a physical examination to rule out any obvious abnormalities. These will be followed by these tests:
Ultrasound. This type of foetal ultrasound is an imaging technique that uses high-frequency sound waves to produce images of a baby in the uterus and targets a suspected problem, such as a development that’s not typical.
Your healthcare provider might use an ultrasound to measure the length of your cervix to determine if you’re at risk of preterm labour. They will also check the position of the placenta to see if normal.
Laboratory tests: urine, and testing for infectious diseases such as HIV and syphilis.
Anomaly ultrasound. This is an ultrasound to detect genetic anomalies in a pregnancy.